
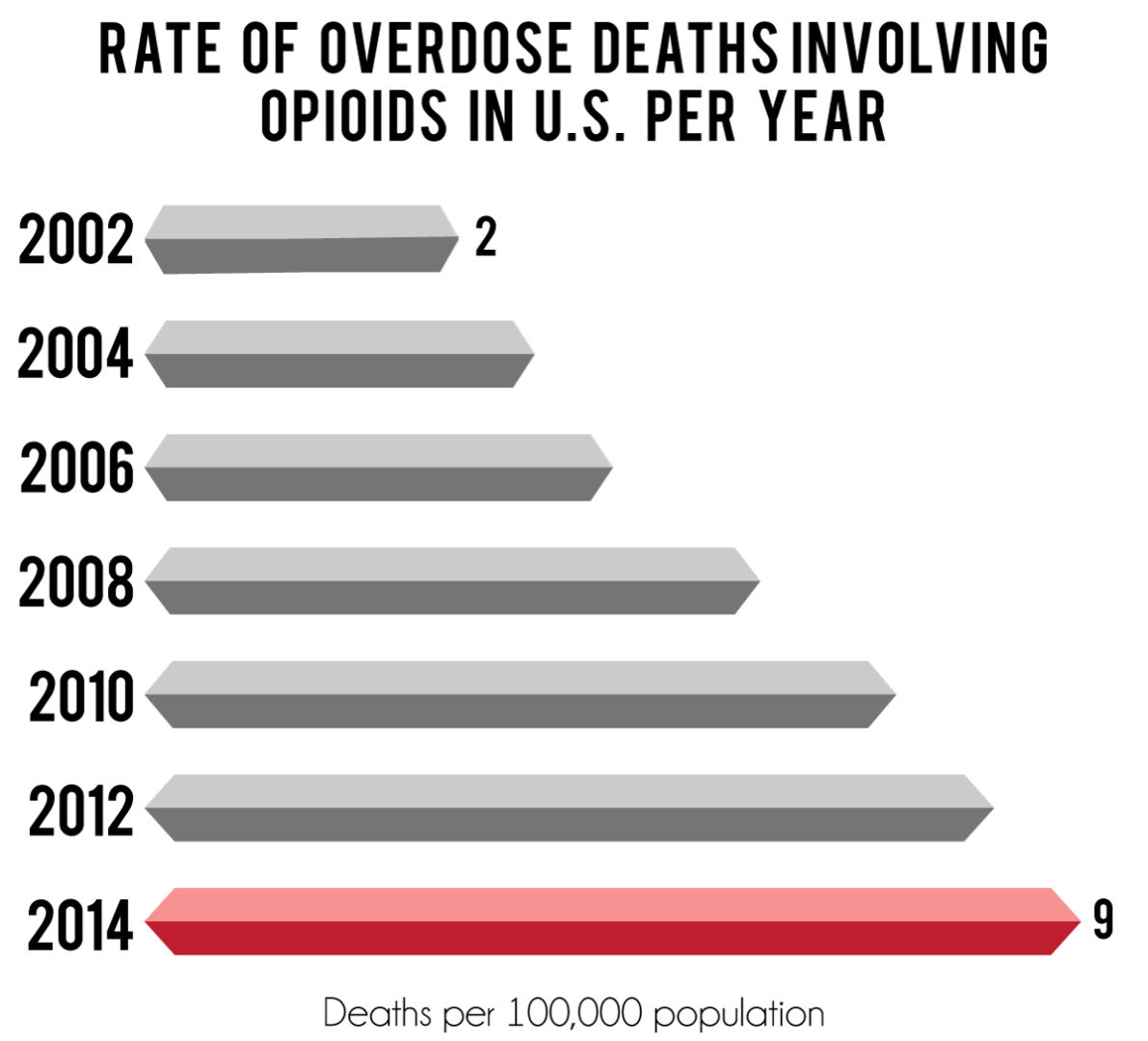
The rise of opioid prescription overdose leads to new guidelines for nurses. | Graphic by Leah Nash/The Cougar
The University of Houston School of Nursing will implement new teaching methods that exclude opioids in the rise of opioid-related overdoses in the U.S.
The Centers for Disease Control and Prevention (CDC) say more than 165,000 people have died from overdoses related to prescription opioids from 1999 to 2014. UH School of Nursing will reshape students’ curriculum based off of the new CDC guidelines regarding using opioids in patient care.
Founding Dean Kathryn Tart said the school has always followed CDC guidelines and it was simply a matter of adding UH’s name to the list.
“We want the public to know that our FNP (Family Nurse Practitioner) program is responsive and practices safely,” Tart said.
Three principles are emphasized among the 12 recommendations in the new guidelines: Non-opioid therapy is preferred for chronic pain outside of active cancer, palliative, and end-of-life care; when opioids are used, the lowest possible effective dosage should be prescribed; and providers should always exercise caution when prescribing opioids.
FNP student Sanjay Abeyadeera said that the guidelines are important, but they have little power in prescribing.
“As an FNP, we have limited prescriptive authority in Texas unless under special circumstances like a specialty or even hospice,” Abeyadeera said.
Associate Dean Kathleen Reeve said the School of Nursing also incorporates prescription guidelines from various organizations including the American Cancer Society and the American Academy of Pain Medicine into their curriculum.
“The inclusion of the CDC’s updated guidelines will provide additional evidence and research to strengthen the case for more focused awareness of the national addiction problem,” Reeve said. “Students will continue to be taught that it is critical to be aware of and incorporate current standards in their practice when prescribing pain medication for acute or chronic pain.”
Reeve said that prescribing habits are not the only factor involved in opioid misuse, and several factors aside from prescribing are contributing to the nationwide epidemic.
“Research indicates that there is a parallel relationship between the availability of prescription opioids through legitimate channels and the diversion and abuse of opioids,” Reeve said. “With the decrease in opioid prescriptions being written over the last few years, there has been an upsurge in the use of low-cost heroin.”
Students within the FNP program are taught Evidence Based Practice (EBP), which is the use of current best evidence in making decisions for patient care. The process allows the practitioner to assess information based on findings and apply the results in practice.
Tart feels that individualized care is an important step to the multi-faceted issue of lowering the number of Americans addicted to prescription drugs.
“Healthcare providers like nurse practitioners and physicians need to assess their patient’s needs to individualize care and provide effective follow-up care,” Tart said.
Although many who abuse opioids do not suffer from acute pain, the School of Nursing is working on ways to help patients who do experience it.
Students are taught the significance of practicing physical therapy, exercising, relaxation techniques and non-opioid pharmacologic therapies such as nonsteroidal anti-inflammatory drugs (NSAIDS) and other medications.
news@thedailycougar.com
—
“School of Nursing changes methods in rise of opioid overdose” was originally posted on The Daily Cougar
